When you or someone you love has been admitted to the hospital for a surgical procedure, you expect to leave healthier. Sadly, some patients develop a healthcare-associated infection (HAI) that leaves them sicker than when they arrived. Bloodstream staph infections are the leading cause of HAI infections in the U.S. When bacteria enter the bloodstream, a staph infection can lead to sepsis or death. According to a new report by the CDC, more than 119,000 Americans suffered from Staphylococcus aureus bloodstream infections in 2017. Nearly 20,000 of these people died.
“Staph infections are a serious threat and can be deadly. U.S. hospitals have made significant progress, but this report tells us that all staph infections must remain a prevention priority for healthcare providers.” Robert Redfield, MD, CDC Director
Are Hospitals Doing Enough to Prevent Staph Infections?
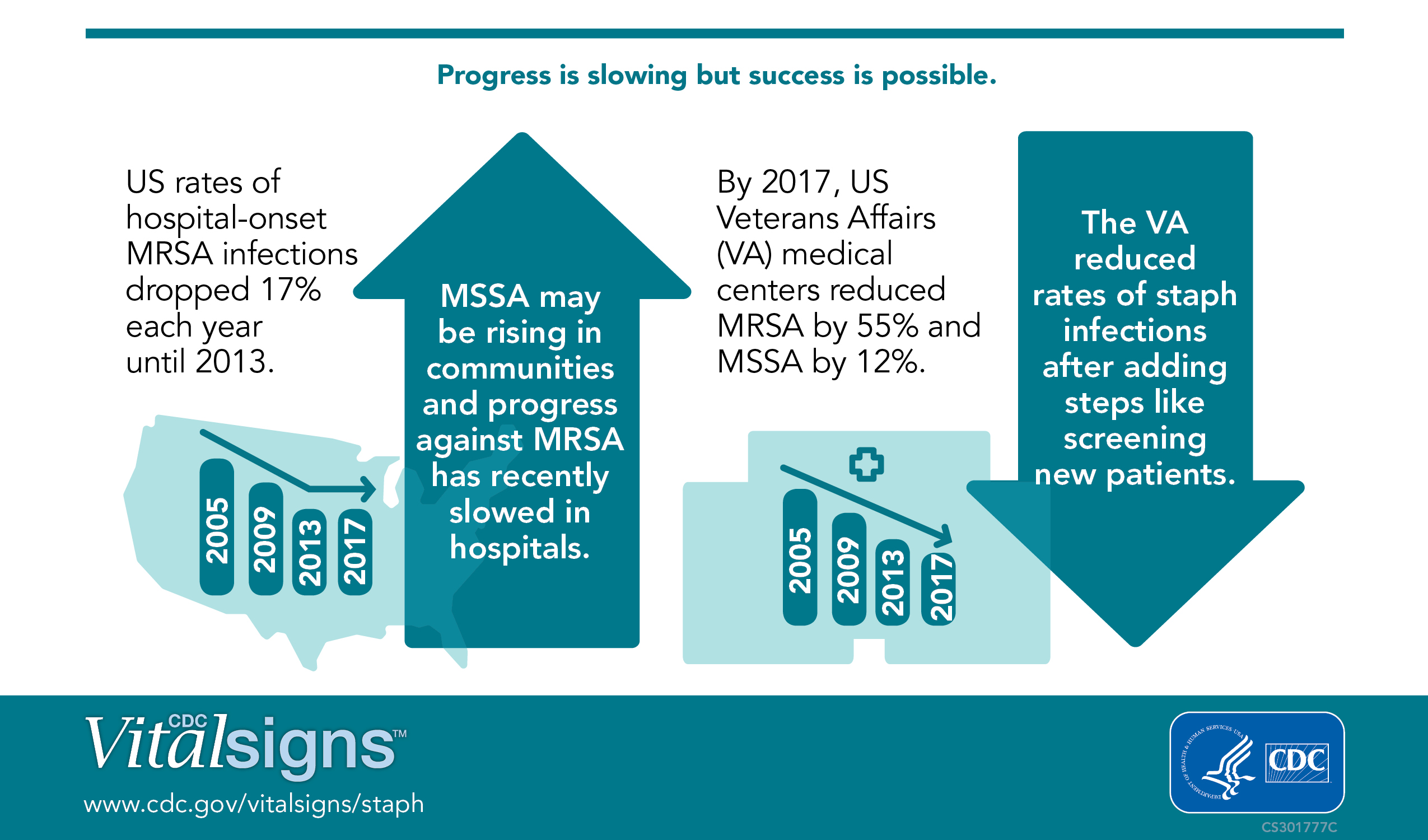
The short answer is, some are and some are not. From 2005-2012, the rate of hospital-onset methicillin-resistant S. aureus (MRSA) infections steadily declined by 17.1% each year. However, that rate of decline has recently stalled. Although all hospitals need to implement strategies to protect patients from MRSA, data from the National Healthcare Safety Network indicates that a relatively small number of hospitals account for a disproportionate number of hospital-onset MRSA infections. The discrepancy could be a result of many factors, including:
- Treating a patient population with a high percentage of patients more prone to infection, like opioid users. According to the CDC’s report, people who inject drugs like opioids are 16 times more likely to develop a serious staph infection than people who do not.
- Failure to implement anti-infection protocols, including Contact Precautions (wearing gloves and gowns), screening high-risk patients and decolonization.
The United States is not on track to meet the 2020 goal of the national HAI Action Plan to reduce hospital-onset MRSA infections by 50%. What needs to be done? According to the CDC’s Deputy Director, Dr. Anne Schuchat, hospitals should:
- Implement the CDC’s recommendations for preventing infections, particularly through Contact Precautions
- Continue to review data
- Find new ways to prevent Staph infections from spreading
The CDC cites the U.S. Veterans Affairs medical centers as an example of a healthcare facility that has been able to continually reduce MRSA infections by implementing patient screening strategies.
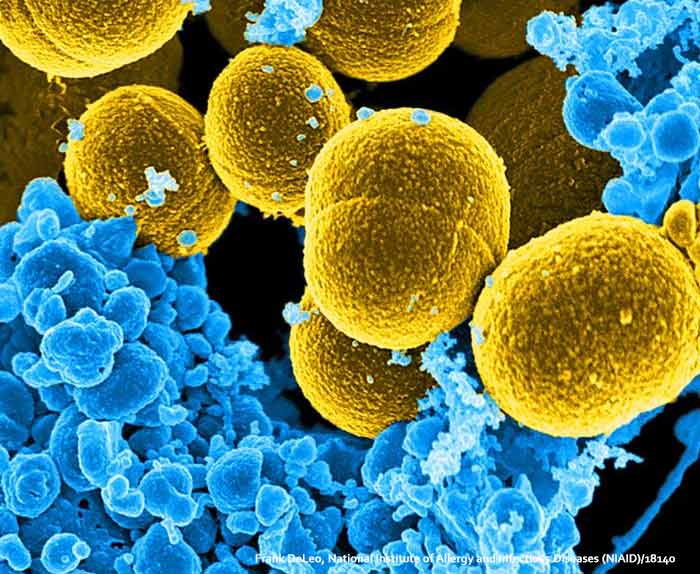
What Causes a Staph Infection?
A staph infection spreads through direct contact with an infected person, by using a contaminated object or by inhaling infected droplets through sneezing or coughing. Staph is either methicillin-resistant (MRSA) or methicillin susceptible (MSSA). Methicillin is a type of penicillin. While MRSA infections are antibiotic-resistant, MSSA infections can be treated with antibiotics. Risk factors for MRSA infections include:
- Being hospitalized
- Having an invasive medical device such as an artificial heart valve or catheter
- Residing in a long-term care facility
- Drug use