A Salmonella outbreak linked to turkey products has sickened dozens of people nationwide. The outbreak has an unusually high hospitalization rate. One person has died.
One recall, for Jennie-O ground turkey, has been issued, but others may follow as the outbreak strain has been found in numerous products and manufacturing facilities.
Health officials say you don’t have to avoid turkey at Thanksgiving this year, but urge all consumers to use care when preparing it.
Turkey Preparation Food Safety Tips
- Whole turkeys should be thawed in the refrigerator in a pan that can hold the juices and stop them from spreading. This is not a quick process. A 16-pound turkey takes four days to thaw in the fridge.
- Another option is to cook the turkey frozen. This takes about 50 percent longer to cook but reduce the risk of spreading harmful bacteria around your kitchen.
- Do not wash your turkey, this just splashes the germs around.
- Wash your hands frequently. If you have handled raw turkey, do not touch something else before washing your hands.
- Use a meat thermometer to make sure the turkey has been cooked to an internal temperature of 165˚ F. Test the turkey in several places.
- Refrigerate leftovers promptly. Cooked turkey can be out at room temperature for a maximum of two hours before bacteria reaches a dangerous level.
A Timeline of Key Events in the Outbreak Investigation
November 20, 2017
The first case-patient in this outbreak begins to experience symptoms of a Salmonella infection which include diarrhea, abdominal cramps, and fever. These symptoms usually develop within six to 72 hours of exposure and last about a week.
February 8, 2018
Raws for Paws of Minneapolis, MN issues a recall raw ground turkey pet food for potential Salmonella contamination. About 4,000 pounds of Ground Turkey Pet Food sold in 5 lb. and 1 lb. chubs are included in the recall which notes that Salmonella can affect animals eating the product and humans who handle it.
February 9, 2018
The Minnesota Department of Health and the Minnesota Department of Agriculture announce a Salmonella outbreak linked to raw turkey pet food that has sickened two children whose pets were served the food. Both children became ill in January 2018. One of them developed osteomyelitis, a painful, serious bone infection.
The U.S. Food and Drug Administration (FDA) also announces the outbreak saying it is working in collaboration with health officials in Minnesota. The FDA stresses the significance of the health risk, saying:
“This outbreak is of particular public health importance because of the potential hazard to both human and animal health. Pets can get sick from Salmonella, but may also be carriers of the bacteria and can infect humans. Pets do not have to be apparently ill to be able to pass Salmonella onto their human companions.”
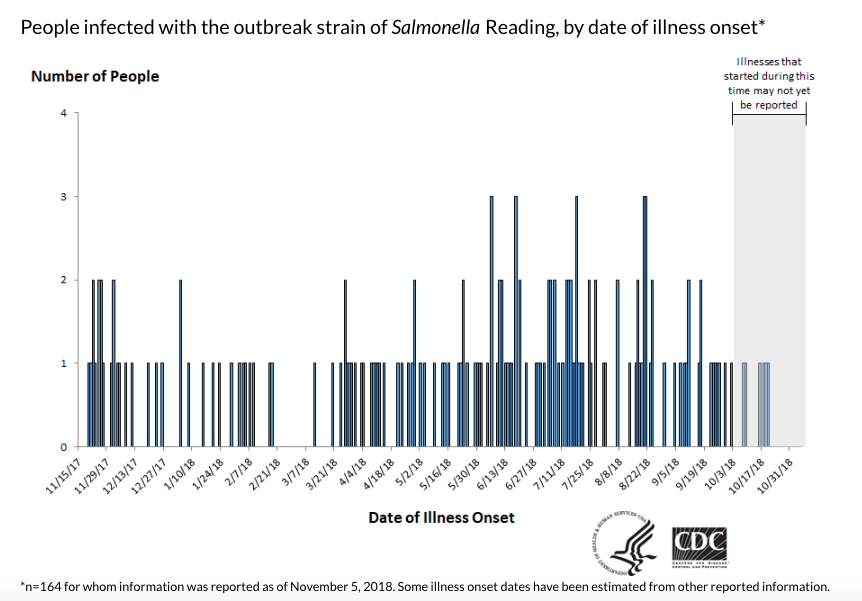
The CDC Announces a Multistate Outbreak
July 19, 2018
The Centers for Disease Control and Prevention (CDC) announces that a Salmonella outbreak linked to raw turkey products has sickened 90 people in 26 states. More than half of them had antibiotic-resistant infections. Forty people were hospitalized, more than twice the average hospitalization rate in a Salmonella outbreak.
By this time, the outbreak strain has already been identified in samples from Raws for Paws raw turkey pet food in Minnesota, from turkeys in several states, and from raw turkey products from 19 slaughterhouses and six processing establishments. The samples collected at these slaughter and processing establishments by USDA FSIS were part of the agency’s routine testing program. The CDC says the outbreak strain’s omnipresence is an indication that this may be an industrywide problem. No recalls are issued.
The case patients, who range in age from one to 91 years old, report onset-of-illness dates ranging from November 20, 2017 to June 29, 2018. Most of them reported eating turkey, prepared whole, in parts or ground before becoming ill. The CDC notes that two of them became sick after pets in their households ate raw ground turkey pet food and three of them worked in a facility that raises or processes turkeys, or lived with someone who did.
The case were reported from the following states: Alaska (1), California (6), Colorado (3), Florida (4), Georgia (2), Hawaii (1), Iowa (2), Illinois (9), Indiana (3), Kansas (1), Kentucky (1), Massachusetts (1), Michigan (2), Minnesota (13), New Jersey (5), New York (8), North Carolina (3), Ohio (2), Oregon (1), Pennsylvania (5), South Carolina (1), South Dakota (1), Tennessee (1), Texas (8), Virginia (3), and Wisconsin (3).
July 27, 2018
The FDA updates its announcement about the Salmonella raw turkey pet food outbreak to say the strain matches the strain of the multi-state turkey Salmonella outbreak.
The Outbreak Turns Deadly
November 8, 2018
The CDC publishes an update on the outbreak. The outbreak has grown and turned deadly. At this point, 164 people in 35 states are sick, according to CDC. About half of them battled antibiotic-resistant infections. Sixty-three people were hospitalized, about twice the average hospitalization rate. One person from California has died.
The case patients, who range in age from less than one to 91 years old, reported onset of illness dates ranging from November 20, 2017, to October 20, 2018. Most of them reported eating turkey, prepared whole, in parts or ground before becoming ill. The CDC notes that a third person who lives in a household where pets were served raw ground turkey pet food is now included, bringing the total number of people who became sick without eating turkey to six.
The case count by state is as follows: Alaska (1), Arizona (1), California (13), Colorado (6), Connecticut (3), Delaware (1), Florida (7), Georgia (2), Hawaii (1), Idaho (1), Iowa (3), Illinois (16), Indiana (3), Kansas (1), Kentucky (1), Maryland (3), Massachusetts (3), Michigan (6), Minnesota (17), Missouri (1), Nebraska (1), New Jersey (8), New York (12), North Carolina (7), North Dakota (2), Ohio (5), Oklahoma (1), Oregon (2), Pennsylvania (8), South Carolina (1), South Dakota (1), Tennessee (1), Texas (12), Virginia (8), and Wisconsin (6).
The USDA has found the outbreak strain in even more places. The outbreak strain has now been found in 22 different slaughterhouses and seven different processing facilities. This is in addition to matches found in samples of raw turkey pet food in Minnesota, in live turkeys in several states and in raw turkey products collected from ill people’s homes. Sixty percent of the samples from animals and food show antibiotic resistance. Again, the CDC says it might be an industry-wide problem. No recalls are issued.
Consumer Groups Urge USDA to Disclose Names
November 13, 2018
The Center for Science in the Public Interest, a nonprofit food safety consumer watchdog group, urges action. CSPI Deputy Director of Regulatory Affairs Sarah Sorscher publishes a statement that read in part:
“The U.S. Department of Agriculture knows more about the turkey products implicated in this outbreak than it is disclosing to the media or the American people. The agency has detected the outbreak strain in samples from raw turkey products from 22 slaughter and 7 processing establishments but has not published their names.
We urge USDA to name these establishments. It is the responsibility of the government to ensure that the turkeys headed for our Thanksgiving tables do not harbor antibiotic-resistant bacteria that have caused human illness and death. And if it can’t do that, it should at least help consumers avoid tainted turkey.”
November 14, 2018
The advocacy arm of Consumer Reports calls on the USDA to release the names of turkey producers, suppliers, and brands linked to the outbreak.
“The USDA should immediately make public which turkey producers, suppliers, and brands are involved in this outbreak — especially with Thanksgiving right around the corner,” Jean Halloran, director of Food Policy Initiatives for Consumer Reports, said in the statement. “This information could save lives and help ensure consumers take the precautions needed to prevent anyone in their home from getting sick.”
Later that day…
The USDA issues a statement outlining its progress in the outbreak investigation that is not posted on its website. (It appears in full below this timeline.) In the statement, the agency pushes back at the consumer groups’ pleas for more information with a terse suggestion that food safety advocates save the “Monday-morning quarterbacking” and leave outbreak investigation to the professionals. “If we had specific products that we could alert consumers to with a Public Health Alert, we would issue one,” the agency said.
November 15, 2018
Congresswoman Rosa DeLauro (D- CT) issues a statement regarding the USDA’s response to the ongoing outbreak. In it, she calls out the agency for attacking the consumer groups and says the agency is putting corporate interests over the health of Americans. It reads in part:
“The public entrusts the USDA to keep our nation’s meat and poultry products safe. That is what makes the ongoing Salmonella outbreak so troubling. Congress and the public have no indication that the USDA is any closer to resolving this outbreak today than they were nearly one year ago when the first illness was reported. Instead of providing more information—like naming implicated plants—the USDA has attacked consumer safety advocates for seeking answers. That is wrong, and it is not the type of behavior a government agency or its employees should be engaged in.”
“This outbreak is just another example of the USDA putting corporate interests over the health of American families. That is why I have long advocated for changes to food safety law that would define antibiotic-resistant Salmonella as an adulterant in poultry products. Congress needs to act on this bill immediately. More than that, with Thanksgiving just one week away, the public deserves transparency from the USDA and to know if their families are being put at risk.”
DeLauro is the author of the Pathogen Reduction and Testing Reform Act which aims to help the USDA better safeguard Americans. A key reform included in the bill would define some Salmonella strains as adulterants in poultry, just as seven strains of E. coli are. This change would subject meat and poultry products contaminated with Salmonella to the USDA’s mandatory recall authority.
Later that day…
Jennie-O Ground Turkey Recall
On November 15, 2018 Jennie- O Turkey Stores Sales issues a recall of more than 91,000 pounds of ground turkey products distributed nationwide. The recall occurs one day after the USDA said if it knew of specific products linked to the outbreak it would issue a Public Health Alert. The agency did not issue a Public Health Alert but did post the recall on its website with an “Editor’s Note” saying that the investigation is ongoing and additional products from additional companies may also be recalled.
The Jennie-O recall includes four products, all bearing the establishment number “P-190” inside the USDA mark of inspection. They are:
- 1-lb. packages of “Jennie-O GROUND TURKEY 93% LEAN | 7% FAT” with “Use by” dates of 10/01/2018 and 10/02/2018.
- 1-lb. packages of “Jennie-O TACO SEASONED GROUND TURKEY” with a “Use by” date of 10/02/2018.
- 1-lb. packages of “Jennie-O GROUND TURKEY 85% LEAN | 15% FAT” with a “Use by” date of 10/02/2018.
- 1-lb. packages of “Jennie-O ITALIAN SEASONED GROUND TURKEY” with a “Use by” date of 10/02/2018.
The recall was issued after public health officials in Arizona found the outbreak strain in unopened Jennie-O brand ground turkey from an ill person’s home.
Jennie-O Outbreak Strain Can be found in 29 plants from 19 Companies
Jennie-O President Steve Lykken includes a statement with the recall information posted on the company’s website. It reads:
“On behalf of the thousands of Jennie-O team members, we were concerned to learn that someone became ill after exposure to Salmonella in a raw turkey product. The turkey industry has been working together for many years to reduce Salmonella. Despite these efforts, this particular Salmonella strain can be found in 29 different manufacturing plants from 19 different companies, according to government agencies. We know the issue of Salmonella isn’t specific to Jennie-O, and to that end, we plan on continuing our leadership role in the effort to reduce Salmonella and educate consumers on how to safely handle and prepare raw turkey and are calling on others in the industry to do the same. We will continue to collaborate on industry best practices with our peers in the turkey industry. As always, turkey remains safe to consume when handled and prepared properly. Jennie-O has information available on its website with step-by-step instructions on how to safely prepare and enjoy turkey.”.
November 16, 2018
Consumer Reports Advocacy issues a statement that describes the recall “a good start” and calls for further action. It says in part:
“The recall is a good start, but considering the millions of turkeys that will be eaten over the holiday, the USDA should give consumers much more information about the results of its ongoing investigation,” said Jean Halloran, Director of Food Policy Initiatives for Consumer Reports. “USDA still hasn’t released the names of the slaughter and processing facilities where it found the outbreak strain through genetic fingerprinting. The government should publicly identify those plants and the brands produced at those facilities. USDA also should give consumers guidance on how to check the label code of a turkey at the grocery store, so they can see if it came from a processing facility where this dangerous Salmonella strain was found.”
November 17, 2018
Jennie O expands the recall to include one additional product and increased amounts of the others. The recall now includes:
- 1-lb. packages of “Jennie-O GROUND TURKEY 93% LEAN | 7% FAT” with “Use by” dates of 10/01/2018 and 10/02/2018.
- 1-lb. packages of “Jennie-O TACO SEASONED GROUND TURKEY” with a “Use by” date of 10/02/2018.
- 1-lb. packages of “Jennie-O GROUND TURKEY 85% LEAN | 15% FAT” with a “Use by” date of 10/02/2018.
- 1-lb. packages of “Jennie-O ITALIAN SEASONED GROUND TURKEY” with a “Use by” date of 10/02/2018.
- 1-lb. packages of “GROUND TURKEY 90% LEAN | 10% FAT” with a “Use by” date of 10/02/2018
November 18, 2018
Hormel Foods Corp. the Austin, MN-based parent company of Jennie-O tells the Associated Press that it owns five of the 29 plants where the outbreak strain was discovered.
Full statement from the USDA FSIS on the status of the turkey Salmonella outbreak issued November 14, 2018
The U.S. Department of Agriculture’s Food Safety and Inspection Service (FSIS), the U.S. Centers for Disease Control (CDC) and state health departments are working together to investigate and bring to an end the outbreak of Salmonella Reading in raw turkey products.
We know that 164 people from 35 states have become ill over the past year from this strain of Salmonella. However, the outbreak strain has been identified in a wide range of samples including raw turkey pet food, raw turkey products, and live turkeys. Our public health partners have interviewed case-patients, and 64% of those patients report eating turkey products. Of the patients who report eating different types and brands of turkey products purchased from different stores, some couldn’t be certain they ate turkey products while others reported handling raw turkey pet food and/or raw turkey or working with live turkeys or living with someone who handled live turkeys. We have interviewed patients, looked at receipts and shopper card data, and tested any product that case-patients still have. All this information is necessary to link back to a supplier or establishment. Despite these ongoing efforts, we do not have the evidence to pinpoint a single common supplier of turkey products. Like any investigation, we are chasing down leads and looking for evidence.
If FSIS had the ability to identify the source of this Salmonella strain, then the agency would immediately recall the items. If we had specific products that we could alert consumers to with a Public Health Alert, we would issue one. At the moment, there is no actionable information for consumers, other than to remind them that this is an ongoing investigation and that consumers should always handle raw turkey carefully and cook it thoroughly to prevent food poisoning. This outbreak is a reminder that raw turkey products can have germs that spread around food preparation areas and can make you sick.
That brings us to the recent demands by special interest groups regarding their accusation that FSIS is withholding information that consumers need to make informed decisions. FSIS takes more than 40,000 raw poultry samples a year in over 6,400 regulated establishments. The agency makes millions of data points available every year, and every month is adding additional reports related to sampling results and individual establishment food safety results – all in an effort to satisfy stakeholder appetite for a more accessible regulatory agency. We will continue to do so. In fact, special interest groups would have no window into the federal government investigation into this outbreak if FSIS hadn’t shared information with them. However, it would be grossly irresponsible and reckless to associate producers with an outbreak investigation, when a link from an establishment to an illness has not been made. It’s also not helpful to consumers. Traceback investigations are conducted in the field through on the groundwork, not Monday morning quarterbacking from the comforts of an urban high rise in New York City or K Street in Washington, D.C., with fundraising pleas attached.
To be abundantly clear, FSIS has NOT identified a source or supplier of the product or products that are making consumers ill, but we continue to work around the clock with our federal and state public health partners to solve this. It is insulting to suggest that the agency would not move forward if we had actionable information. FSIS is a public health agency that moves forward when science can serve as the foundation of our action plan—not when emotion or pressure from for-profit industry or special interest groups demand it.
As families start their holiday plans they may be wondering what this means for them. The answer is simple. Salmonella is prevalent and can be present in raw meat and poultry and in live poultry – no raw meat or poultry is sterile. Consumers can protect themselves by cooking their turkey, other poultry products, and meat thoroughly. The cooking process kills Salmonella. No one should be eating partially cooked or raw turkey. Additionally, it is essential that people wash their hands after handling raw poultry, meat, and pet food to avoid cross-contamination of other foods, spice containers, or kitchen surfaces.
FSIS will continue to work with our public health partners to release information as it becomes available and will take action when we have the evidence. We are following up on every lead and working with our public health partners to find the source of the Salmonella Reading. In the meantime, it’s important that consumers know they can purchase and safely consume these products. The U.S. has the safest food supply in the world and USDA works every day to ensure it.